What the New Rules on Birth Control Mean for You
Posted by URGE Staff
May 15, 2015
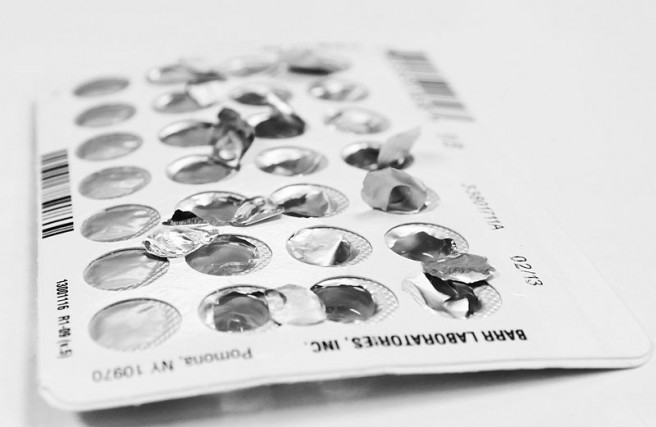 photo by Bryancalabro, via Wikimedia
photo by Bryancalabro, via Wikimedia
You may have seen the buzz this week about the new guidance for birth control under the Affordable Care Act. This is exciting news! Health and Human Services (HHS), the agency that creates the rules to make sure the Affordable Care Act is implemented correctly, just published a set of FAQs that clarify for insurance provider’s that yes – they must cover birth control without a co-payment.
A recent study by the National Women’s Law Center and the Kaiser Family Foundation found that many folks were having a hard time getting the birth control that their doctor prescribed without a co-pay. Frequently, insurance would not cover the NuvaRing or the patch because they already covered hormonal birth control in the form of the pill. The new rules released by HHS make it clear that insurers have to cover at least one form of birth control in all eighteen categories that the FDA has approved in non-grandfathered plans (check out this article that is helpful in explaining what a grandfathered plan is). I know that can sound a little wonky, but take a look at this helpful chart from the FDA to see all covered forms of birth control. Additionally, the guidance makes it clear that if you are a dependent on your parent’s health insurance, the insurer must still cover your birth control.
The new rules also state that all of the services related to your birth control must be covered. For example, the appointment to insert an IUD and the follow up appointment must be fully covered by your insurance. However, insurers are still allowed to practice what is called “medical management.” For instance, plans can have policies that encourage using generic forms of contraception over brand name by requiring co-pays for brand name drugs. But if there is a medical reason why you need the brand name, an insurer must cover it, but may require you to go through an appeal process. It is important to keep in mind that because the regulations allow for medical management and require insurers to only cover one kind of birth control in each category – you may have to jump through a few hoops to get the birth control you want without a co-pay. That being said, the new guidance is welcome news and should be a powerful tool when and if you need to advocate for yourself with your insurer.
One of the most exciting parts of the new rules is a clarification on what preventative care must be covered for transgender folks without a co-pay. Because the recommended preventative services are classified by sex, this clarifying regulation states that if a provider determines that a service is medically necessary for an individual and that service falls within the “preventative service” category then the insurer must cover it without co-pay. The guidance says explicitly “the plan or issuer must provide coverage for the recommended preventive service, without cost sharing, regardless of sex assigned at birth, gender identity, or gender of the individual otherwise recorded by the plan or issuer.”
This is all great news and should make it easier and more streamlined for folks to access the reproductive health services they need, regardless of their gender identity.
Keep in mind that the new rules do not go into effect for 60 days after the published guidelines – which was May 11, 2015. If you still run into problems accessing your birth control, you can reach out the to the CoverHer line through the National Women’s Law Center.
Written by Kelsey Ryland, URGE Law & Policy Fellow
Leave a Reply
You must be logged in to post a comment.

